Investigative Report, Investigative story report
Achieved$0.00
Target$0.00
0
%
Pledged So Far
 In Nigeria, a silent crisis was unfolding, hidden within the chaos caused by the banknote redesign. What was meant to combat counterfeiting and strengthen the economy had unforeseen consequences that left pregnant women in dire straits. In this report, ADETUTU SOBOWALE writes on the sufferings and how the naira debacle pushed pregnant women to the brink.
The shortage of cash in February 2023 truncated many businesses and livelihoods in Nigeria. This affected many and led millions of the nation's residents to protest. Pregnant women, just like every average Nigerian, experienced the naira scarcity. Bola Onibuore, a resident of Ajegunle, Sango-Ota in Ado-Odo Ota Local Government Area of Ogun State was badly affected. The naira crunch posed a threat to Onibuore and her unborn child being her first pregnancy. The lives of the mother and child depended on getting scarce new naira notes to eat, to drink and to buy medicine. Onibuore became restless when she could not meet with her doctor for prenatal consultation service at the health centre in Sango-Ota area where she had registered. Contrary to medical laws that place lives above money, the lack of the new naira notes means no access to a medical doctor by pregnant women like Onibuore.
In the physician oath also known as the Geneva Declaration, doctors pledge to practise their profession with integrity and respect; to prioritise the health of their patients above everything else and maintain a deep preference for human life, even in challenging circumstances; and they also commit to using their medical knowledge according to humanitarian laws and principle. Every doctor solemnly swears this oath during the "Oath-taking Ceremony" when they become newly qualified physicians. However, despite its apparent simplicity, many pregnant women were left to wallow in pain and hardship due to the unavailability of naira.
Onibuore was caught in the cash shortage failure causing distress and denial of healthcare services to her and many pregnant women across the country. She was turned down at the hospital after pleading with the health workers to accept old notes from her as she witnessed some other expectant mothers leave the healthcare centre unattended to, dejected and disappointed. The request of the 30-year-old was turned down not because her family had no funds, but, like millions of Nigerians, their monies were trapped in the bank. Pregnant women like Onibuore were denied access to healthcare services for over two months because they could not get the scarce newly redesigned notes from banks. “It was a big mess. On my consecutive visits, the PHC became scanty as people stopped coming since they would not be attended to by the health workers. This decision of the health workers scares me a lot. I'm still battling with the fear of the effect of missing the antenatal care on my child and even labour,” Onibuore, the small-scale business owner said. She narrated how expectant mothers were disrespected by a health provider during one of her visits, "When I went back with the requested new naira notes, I saw a heavily pregnant woman being shouted at and denied access to healthcare service because she had no new notes. This was so unpleasant. Who knows what could have happened to the woman by now?” she added.
A ‘frustrated' policy.
In Nigeria, a silent crisis was unfolding, hidden within the chaos caused by the banknote redesign. What was meant to combat counterfeiting and strengthen the economy had unforeseen consequences that left pregnant women in dire straits. In this report, ADETUTU SOBOWALE writes on the sufferings and how the naira debacle pushed pregnant women to the brink.
The shortage of cash in February 2023 truncated many businesses and livelihoods in Nigeria. This affected many and led millions of the nation's residents to protest. Pregnant women, just like every average Nigerian, experienced the naira scarcity. Bola Onibuore, a resident of Ajegunle, Sango-Ota in Ado-Odo Ota Local Government Area of Ogun State was badly affected. The naira crunch posed a threat to Onibuore and her unborn child being her first pregnancy. The lives of the mother and child depended on getting scarce new naira notes to eat, to drink and to buy medicine. Onibuore became restless when she could not meet with her doctor for prenatal consultation service at the health centre in Sango-Ota area where she had registered. Contrary to medical laws that place lives above money, the lack of the new naira notes means no access to a medical doctor by pregnant women like Onibuore.
In the physician oath also known as the Geneva Declaration, doctors pledge to practise their profession with integrity and respect; to prioritise the health of their patients above everything else and maintain a deep preference for human life, even in challenging circumstances; and they also commit to using their medical knowledge according to humanitarian laws and principle. Every doctor solemnly swears this oath during the "Oath-taking Ceremony" when they become newly qualified physicians. However, despite its apparent simplicity, many pregnant women were left to wallow in pain and hardship due to the unavailability of naira.
Onibuore was caught in the cash shortage failure causing distress and denial of healthcare services to her and many pregnant women across the country. She was turned down at the hospital after pleading with the health workers to accept old notes from her as she witnessed some other expectant mothers leave the healthcare centre unattended to, dejected and disappointed. The request of the 30-year-old was turned down not because her family had no funds, but, like millions of Nigerians, their monies were trapped in the bank. Pregnant women like Onibuore were denied access to healthcare services for over two months because they could not get the scarce newly redesigned notes from banks. “It was a big mess. On my consecutive visits, the PHC became scanty as people stopped coming since they would not be attended to by the health workers. This decision of the health workers scares me a lot. I'm still battling with the fear of the effect of missing the antenatal care on my child and even labour,” Onibuore, the small-scale business owner said. She narrated how expectant mothers were disrespected by a health provider during one of her visits, "When I went back with the requested new naira notes, I saw a heavily pregnant woman being shouted at and denied access to healthcare service because she had no new notes. This was so unpleasant. Who knows what could have happened to the woman by now?” she added.
A ‘frustrated' policy.
 Former Central Bank of Nigeria Governor Godwin Emiefele
In October 2022, the Central Bank of Nigeria announced the resignation of the N200, N500, and N1,000 banknotes. The action was in response to a request from the Federal Government through Godwin Emiefele the former apex bank Governor who stated that the new banknotes would begin circulation on 15 December 2022, alongside the old banknotes which would remain legal tender until 31 January 2023. According to Emefiele, the redesign will enhance control over the naira, manage inflation, combat counterfeiting, and address ransom payments.
Former Central Bank of Nigeria Governor Godwin Emiefele
In October 2022, the Central Bank of Nigeria announced the resignation of the N200, N500, and N1,000 banknotes. The action was in response to a request from the Federal Government through Godwin Emiefele the former apex bank Governor who stated that the new banknotes would begin circulation on 15 December 2022, alongside the old banknotes which would remain legal tender until 31 January 2023. According to Emefiele, the redesign will enhance control over the naira, manage inflation, combat counterfeiting, and address ransom payments.
 Former Minister of Finance Zainab Ahmed
Nigerian were outraged with lack of currency in circulation. Hunger was looming. The Minister of Finance, budget and national planning Zainab Ahmed during the naira redesign raised alarm and expressed concerns about the impact of the policy on the economy. Executive Governors called for a halt to the policy, citing its negative impact on Nigerians. The Supreme Court and the judiciary arm nullified the ban on the use of the old N200, N500, and N1000 banknotes as legal tenders. Due to public outcry and lack of awareness, the CBN initiated a cash swap program to exchange old notes for redesigned ones.
Health workers cared less.
Mutiat Adeoye, a resident of Abule Oloni, Lantoro, Abeokuta in Ogun State was visiting the Sacred Heart hospital in Abeokuta, the state capital as she was due for delivery. She was informed by health workers at the centre to get her delivery kits from home. However, the story changed when she returned to the facility as she was not attended to despite being in labour because she did not have the new notes. "I pleaded but it fell on the deaf ears of the attendant. She insisted on the new notes which I only had N5,000 out of the over N100,000 payment I had to make. I was traumatised and scared of what could happen to me if my baby was not delivered. I was in severe pain but the health worker cared less," she lamented. An obstetrician, Dr. Aisha Abdulsalam, emphasised that antenatal care is crucial for both first-time mothers and those with previous pregnancies due to the unique challenges each pregnancy can present. Abdulsalam added that to ensure comprehensive care, the World Health Organisation recommends a minimum of four antenatal visits for pregnant women. The effect of lack of access to antenatal care for pregnant women could affect the mental well-being of pregnant women according to Abdulsalam, "If a woman that understands the gravity of her care and understands why she needs that care cannot access it, it can lead to a lot of emotional stress, psychological stress that would be associated with that lack, and yet the woman can go into depression."
In Kaduna state, a pregnant woman lost her life due to the unavailability of the new naira notes as hospitals insisted that patients pay with the new notes. She went into labour but was rejected, turned away by the hospital because her husband could not make a payment due to the new naira scarcity. According to Daily Trust, she bled to death and died at home after giving birth.
Mortality at high rate
Nigeria has an increase in maternal mortality rate with 576 deaths recorded per 100,000 live births, and 262,000 newborns losing their lives annually according to United Nations Children's Fund (UNICEF). This placed the burden of over one-third of global maternal deaths on Nigeria's shoulders. 40 million Nigerian women of reproductive age between 15 and 49 years face a extremely high level of health challenges related to childbirth. Backing up this worrisome statistic, Abdulsalam noted that inadequate access to antenatal care services and reliance on untrained birth attendants are critical factors contributing to the health risks faced by pregnant women in Nigeria. Others include lack of access to adequate maternal healthcare services, severe gestational diabetes, clamped disconnection in pregnancy, postpartum haemorrhage, and death adding that seeking care from non-trained birth attendants is unsafe for both mother and child. "In situations where women seek care in facilities that cannot timely identify complications, it can result in severe consequences. These complications include severe gestational diabetes, clamp disconnection in pregnancy, postpartum haemorrhage, and even maternal death. There is also risk of pregnancy loss, including miscarriages, abortion, and intrauterine foetal demise” Abdulsalam explained further that appropriate care must be planned when pregnant women develop complications. “It is vital to provide appropriate care for women who develop these complications, as the ability to anticipate and manage them is of utmost importance. If women are unable to access the necessary care due to the new naira policy, the potential for adverse outcomes increases. There is room for easing the point of the failed machine with their card in (some) hospitals, they could do a transfer and that was quite the order of the day in the hospital then, but I know some people will reject it."
Over 4.5 million women and babies die every year during pregnancy and childbirth.
In May 2023, the World Health Organisation (WHO) raised alarm that a pregnant woman or newborn baby dies every seven seconds for eight years. WHO in a publication titled ‘Improving maternal and newborn health and survival and reducing stillbirth,’ identified decreasing investments in the health sector as the cause for the rise in maternal and newborn deaths. The report shows that progress in improving survival has stalled since 2015, with around 290,000 maternal deaths, 1.9 million stillbirths, and 2.3 million newborn deaths each year.
Countries with the largest numbers of deaths in 2020
Former Minister of Finance Zainab Ahmed
Nigerian were outraged with lack of currency in circulation. Hunger was looming. The Minister of Finance, budget and national planning Zainab Ahmed during the naira redesign raised alarm and expressed concerns about the impact of the policy on the economy. Executive Governors called for a halt to the policy, citing its negative impact on Nigerians. The Supreme Court and the judiciary arm nullified the ban on the use of the old N200, N500, and N1000 banknotes as legal tenders. Due to public outcry and lack of awareness, the CBN initiated a cash swap program to exchange old notes for redesigned ones.
Health workers cared less.
Mutiat Adeoye, a resident of Abule Oloni, Lantoro, Abeokuta in Ogun State was visiting the Sacred Heart hospital in Abeokuta, the state capital as she was due for delivery. She was informed by health workers at the centre to get her delivery kits from home. However, the story changed when she returned to the facility as she was not attended to despite being in labour because she did not have the new notes. "I pleaded but it fell on the deaf ears of the attendant. She insisted on the new notes which I only had N5,000 out of the over N100,000 payment I had to make. I was traumatised and scared of what could happen to me if my baby was not delivered. I was in severe pain but the health worker cared less," she lamented. An obstetrician, Dr. Aisha Abdulsalam, emphasised that antenatal care is crucial for both first-time mothers and those with previous pregnancies due to the unique challenges each pregnancy can present. Abdulsalam added that to ensure comprehensive care, the World Health Organisation recommends a minimum of four antenatal visits for pregnant women. The effect of lack of access to antenatal care for pregnant women could affect the mental well-being of pregnant women according to Abdulsalam, "If a woman that understands the gravity of her care and understands why she needs that care cannot access it, it can lead to a lot of emotional stress, psychological stress that would be associated with that lack, and yet the woman can go into depression."
In Kaduna state, a pregnant woman lost her life due to the unavailability of the new naira notes as hospitals insisted that patients pay with the new notes. She went into labour but was rejected, turned away by the hospital because her husband could not make a payment due to the new naira scarcity. According to Daily Trust, she bled to death and died at home after giving birth.
Mortality at high rate
Nigeria has an increase in maternal mortality rate with 576 deaths recorded per 100,000 live births, and 262,000 newborns losing their lives annually according to United Nations Children's Fund (UNICEF). This placed the burden of over one-third of global maternal deaths on Nigeria's shoulders. 40 million Nigerian women of reproductive age between 15 and 49 years face a extremely high level of health challenges related to childbirth. Backing up this worrisome statistic, Abdulsalam noted that inadequate access to antenatal care services and reliance on untrained birth attendants are critical factors contributing to the health risks faced by pregnant women in Nigeria. Others include lack of access to adequate maternal healthcare services, severe gestational diabetes, clamped disconnection in pregnancy, postpartum haemorrhage, and death adding that seeking care from non-trained birth attendants is unsafe for both mother and child. "In situations where women seek care in facilities that cannot timely identify complications, it can result in severe consequences. These complications include severe gestational diabetes, clamp disconnection in pregnancy, postpartum haemorrhage, and even maternal death. There is also risk of pregnancy loss, including miscarriages, abortion, and intrauterine foetal demise” Abdulsalam explained further that appropriate care must be planned when pregnant women develop complications. “It is vital to provide appropriate care for women who develop these complications, as the ability to anticipate and manage them is of utmost importance. If women are unable to access the necessary care due to the new naira policy, the potential for adverse outcomes increases. There is room for easing the point of the failed machine with their card in (some) hospitals, they could do a transfer and that was quite the order of the day in the hospital then, but I know some people will reject it."
Over 4.5 million women and babies die every year during pregnancy and childbirth.
In May 2023, the World Health Organisation (WHO) raised alarm that a pregnant woman or newborn baby dies every seven seconds for eight years. WHO in a publication titled ‘Improving maternal and newborn health and survival and reducing stillbirth,’ identified decreasing investments in the health sector as the cause for the rise in maternal and newborn deaths. The report shows that progress in improving survival has stalled since 2015, with around 290,000 maternal deaths, 1.9 million stillbirths, and 2.3 million newborn deaths each year.
Countries with the largest numbers of deaths in 2020
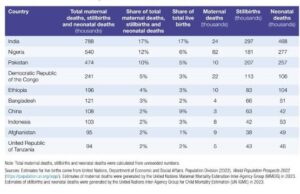
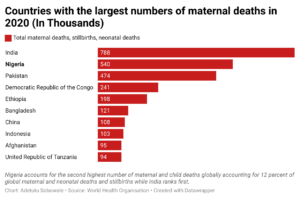 The report further highlighted that over 4.5 million women and babies die every year during pregnancy, childbirth, or the first weeks after birth due to preventable or treatable causes. Nigeria accounts for the second highest number of maternal and child deaths globally with 12 percent of global maternal and neonatal deaths and stillbirths. This figure would have increased during the Naira crisis owing to the attitudes of health practitioners towards expectant mothers.
Violation Of Human Rights
WHO described the loss of life of any woman or young girl while they are pregnant or giving birth as a grave infringement upon their basic human rights. The body said the situation underscores the pressing requirement to expand the availability of high-quality sexual and reproductive health services as an integral part of comprehensive healthcare, particularly in areas where maternal mortality rates have remained stagnant or increased in recent times. Julitta Onabanjo a director at the United Nations Population Fund, emphasised that the death of any woman or young girl during pregnancy or childbirth is a serious violation of their human rights. Onabanjo stressed that these deaths underscore the pressing requirement to expand access to high-quality sexual and reproductive health services within the framework of universal health coverage and primary healthcare. This need is particularly critical in communities where maternal mortality rates have remained stagnant or even increased in recent years. “We must take a human rights and gender transformative approach to address maternal and newborn mortality, and it is vital that we stamp out the underlying factors which give rise to poor maternal health outcomes like socio-economic inequalities, discrimination, poverty, and injustice,” she said. Onabanjo added that women and babies must have quality and affordable healthcare before, during, and after childbirth as well as access to family planning services to increase survival rates.
The Universal Declaration of Human Rights acknowledges the right to life and the highest possible standard of physical and mental health. By denying pregnant women access to healthcare, their lives and well-being are put at risk. Adequate prenatal care is crucial to ensure the health of both the mother and the unborn child, reducing the chances of complications, disabilities, and even maternal and infant mortality. The International Covenant on Economic, Social, and Cultural Rights ICESCR, recognises the right to social security including access to healthcare.
Enforce Universal Healthcare coverage - Health worker urges government.
Abdusalam, while speaking with this reporter noted that universal healthcare coverage plays a significant role in preventing delays in seeking care and reducing the burden of out-of-pocket expenses, which often discourage women from seeking timely medical assistance. She urged the government at all levels to enforce Universal Healthcare coverage. "One of the ways to make delivery easy for women in hospitals is to enforce Universal Healthcare coverage. That has helped women access care all over the world because out-of-pocket payment is currently quite expensive and it is still going to be more expensive, especially with the current financial regulations," she said. To ensure that every woman, regardless of financial constraints, has access to quality healthcare, Abdusalam stressed the urgent need for the government to support subsidised maternal healthcare. "It is something that requires support from the government to subsidise their care so that whether there is a cash crunch or not, every woman has this assurance that when they get to the healthcare centres, they can access care and they don't have to be out of pocket," she said.
Government’s reaction.
The report further highlighted that over 4.5 million women and babies die every year during pregnancy, childbirth, or the first weeks after birth due to preventable or treatable causes. Nigeria accounts for the second highest number of maternal and child deaths globally with 12 percent of global maternal and neonatal deaths and stillbirths. This figure would have increased during the Naira crisis owing to the attitudes of health practitioners towards expectant mothers.
Violation Of Human Rights
WHO described the loss of life of any woman or young girl while they are pregnant or giving birth as a grave infringement upon their basic human rights. The body said the situation underscores the pressing requirement to expand the availability of high-quality sexual and reproductive health services as an integral part of comprehensive healthcare, particularly in areas where maternal mortality rates have remained stagnant or increased in recent times. Julitta Onabanjo a director at the United Nations Population Fund, emphasised that the death of any woman or young girl during pregnancy or childbirth is a serious violation of their human rights. Onabanjo stressed that these deaths underscore the pressing requirement to expand access to high-quality sexual and reproductive health services within the framework of universal health coverage and primary healthcare. This need is particularly critical in communities where maternal mortality rates have remained stagnant or even increased in recent years. “We must take a human rights and gender transformative approach to address maternal and newborn mortality, and it is vital that we stamp out the underlying factors which give rise to poor maternal health outcomes like socio-economic inequalities, discrimination, poverty, and injustice,” she said. Onabanjo added that women and babies must have quality and affordable healthcare before, during, and after childbirth as well as access to family planning services to increase survival rates.
The Universal Declaration of Human Rights acknowledges the right to life and the highest possible standard of physical and mental health. By denying pregnant women access to healthcare, their lives and well-being are put at risk. Adequate prenatal care is crucial to ensure the health of both the mother and the unborn child, reducing the chances of complications, disabilities, and even maternal and infant mortality. The International Covenant on Economic, Social, and Cultural Rights ICESCR, recognises the right to social security including access to healthcare.
Enforce Universal Healthcare coverage - Health worker urges government.
Abdusalam, while speaking with this reporter noted that universal healthcare coverage plays a significant role in preventing delays in seeking care and reducing the burden of out-of-pocket expenses, which often discourage women from seeking timely medical assistance. She urged the government at all levels to enforce Universal Healthcare coverage. "One of the ways to make delivery easy for women in hospitals is to enforce Universal Healthcare coverage. That has helped women access care all over the world because out-of-pocket payment is currently quite expensive and it is still going to be more expensive, especially with the current financial regulations," she said. To ensure that every woman, regardless of financial constraints, has access to quality healthcare, Abdusalam stressed the urgent need for the government to support subsidised maternal healthcare. "It is something that requires support from the government to subsidise their care so that whether there is a cash crunch or not, every woman has this assurance that when they get to the healthcare centres, they can access care and they don't have to be out of pocket," she said.
Government’s reaction.
 Ogun State Commissioner for Health Dr Tomi Coker
When contacted, the Ogun State Commissioner for Health, Dr Tomi Coker, said to cushion the effect of the economic downturn on pregnant women, the state launched an initiative called Ibidero (childbirth has become easier) in the early months of 2023 but did not state the exact month it was initiated. Coker said the initiative was to ensure safety and affordable care for pregnant women and reduce maternal mortality rate across the state. “Ibidero which translates to ‘childbirth has become easier’ in our local dialect, was conceived to address the critical healthcare needs of pregnant women from economically disadvantaged backgrounds. Ibidero is a ‘Vulnerable Group Health Insurance Scheme’, implemented by the Ogun State Health Insurance Agency (OGSHIA). The program which was launched in the early months of this year, with approval to cater for 3,000 beneficiaries across all LGAs of Ogun State, has had a profoundly positive impact on the lives of indigent pregnant women within our communities. With the recent approval by His Excellency, the program is currently being scaled up to cover an additional 15,000 pregnant women across the state, serving as a palliative measure for pregnant women by the government during this hard financial time” Coker said Ibidero will ensure that pregnant women who face financial constraints receive the best possible care during their pregnancy and childbirth, thereby reducing maternal mortality rates, promoting safer deliveries, ensuring a healthier start for newborns and improving the well-being of our citizens.
This report was produced with the support of the Women Radio Centre through the MacArthur Foundation.
Ogun State Commissioner for Health Dr Tomi Coker
When contacted, the Ogun State Commissioner for Health, Dr Tomi Coker, said to cushion the effect of the economic downturn on pregnant women, the state launched an initiative called Ibidero (childbirth has become easier) in the early months of 2023 but did not state the exact month it was initiated. Coker said the initiative was to ensure safety and affordable care for pregnant women and reduce maternal mortality rate across the state. “Ibidero which translates to ‘childbirth has become easier’ in our local dialect, was conceived to address the critical healthcare needs of pregnant women from economically disadvantaged backgrounds. Ibidero is a ‘Vulnerable Group Health Insurance Scheme’, implemented by the Ogun State Health Insurance Agency (OGSHIA). The program which was launched in the early months of this year, with approval to cater for 3,000 beneficiaries across all LGAs of Ogun State, has had a profoundly positive impact on the lives of indigent pregnant women within our communities. With the recent approval by His Excellency, the program is currently being scaled up to cover an additional 15,000 pregnant women across the state, serving as a palliative measure for pregnant women by the government during this hard financial time” Coker said Ibidero will ensure that pregnant women who face financial constraints receive the best possible care during their pregnancy and childbirth, thereby reducing maternal mortality rates, promoting safer deliveries, ensuring a healthier start for newborns and improving the well-being of our citizens.
This report was produced with the support of the Women Radio Centre through the MacArthur Foundation.